CAR T-cell therapy, an innovative approach to treating certain types of cancer, relies on the genetic modification of a patient's immune cells to target and destroy cancer cells. This complex process requires highly specialized laboratory procedures, and it is essential to prioritize the safety of the modified cells, the patient, and the healthcare professionals involved.
This article delves into the CAR T-cell genetic modification process, the crucial role contamination control plays, and the critical role of Personal Protective Equipment (PPE) in maintaining a secure environment.
The CAR T-Cell Genetic Modification Process
1. Collection of T Cells
- T cells are collected via leukapheresis, a process similar to blood donation.
- Leukapheresis isolates T cells from other blood components.
- Sterile conditions prevent contamination at this critical stage.
2. Isolation and Activation
- T cells are isolated and activated in a controlled lab environment.
- Cells are cultured and prepared for modification.
3. Genetic Modification
- A Chimeric Antigen Receptor (CAR) gene is introduced to enable cancer targeting.
- Lentiviral or retroviral vectors are used to deliver the gene safely.
- Contamination control ensures modification integrity.
4. Expansion
- Modified T cells are expanded to therapeutic levels.
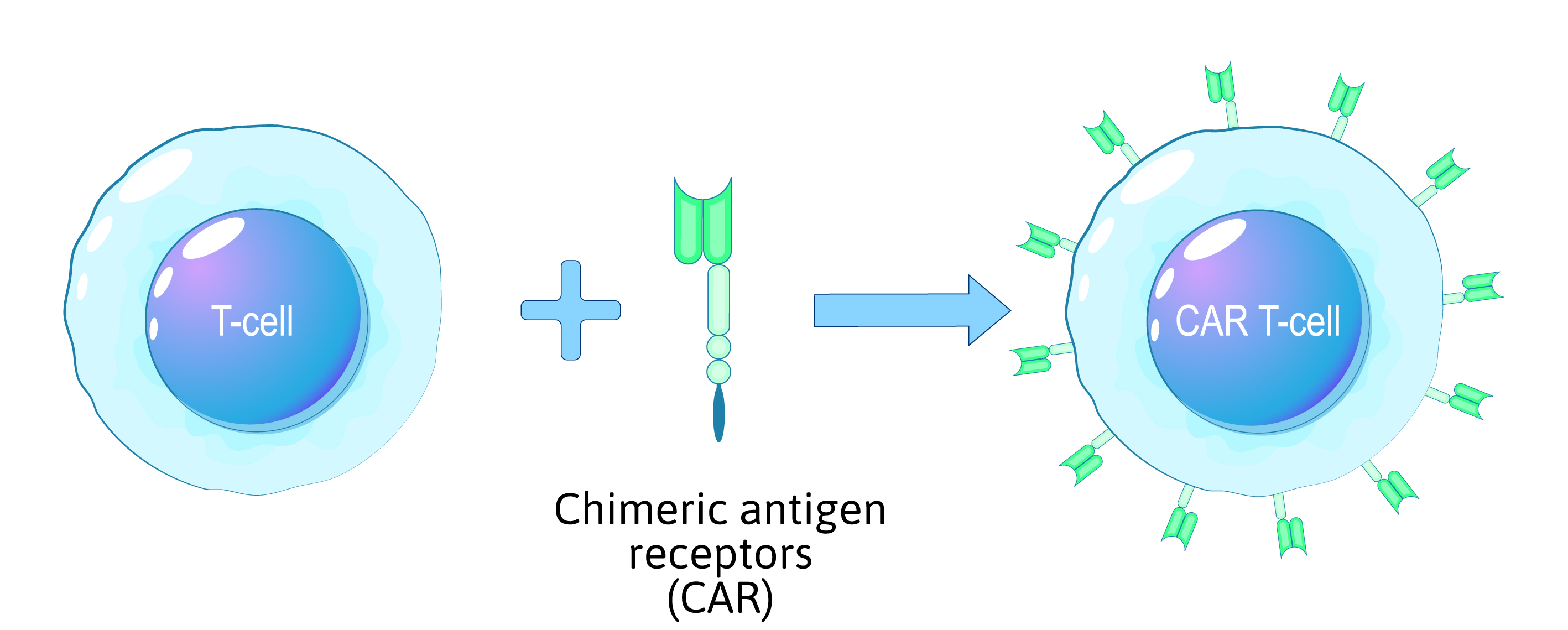 Figure 1: Overview of the CAR T-cell reprogramming process.
Figure 1: Overview of the CAR T-cell reprogramming process.
5. Quality Control
- Cells are tested for purity, viability, and effectiveness.
- Only the highest-quality cells proceed to the next step.
6. Infusion into the Patient
- The modified CAR T cells are infused into the patient.
- This marks the start of a targeted immune response against cancer.
Contamination Control Measures
Effective contamination control is imperative throughout the CAR T-cell genetic modification process to maintain the integrity of the therapy and ensure the safety of both patients and laboratory personnel. Key contamination control measures include:
1. Sterile Techniques:
Laboratory personnel must strictly adhere to sterile techniques, including handwashing, gowning, and gloving, to ensure that all equipment and materials used are sterile.
2. Biological Safety Cabinets (BSCs):
Genetic modification of cells takes place within Class II Biological Safety Cabinets, which provide a controlled and sterile environment. These cabinets help contain potential contaminants and protect laboratory workers.
3. Cleanroom Facilities:
CAR T-cell production often occurs in ISO-class cleanroom facilities, which are specifically designed to maintain high levels of cleanliness and control particulate contamination.
4. Isolation Barriers:
Physical isolation barriers, such as laminar flow hoods and closed systems, are used to prevent contamination during cell manipulation and culture processes.
5. Routine Monitoring:
Regular monitoring of laboratory environments for air quality, surface contamination, and microbial presence is essential to identify and address potential sources of contamination promptly. Common monitoring tools include particle counters and microbial samplers.
6. Waste Disposal:
Proper disposal of waste materials, including potentially contaminated equipment and biological waste, is crucial to prevent contamination. The disposal of contaminated materials, including sharps, is vital to prevent any accidental exposure to personnel.



